Running research topics:
Mrg receptors in GI neuro-immune communication
Mas-related gene receptors as new mediators of gastro-intestinal neuro-immune communication
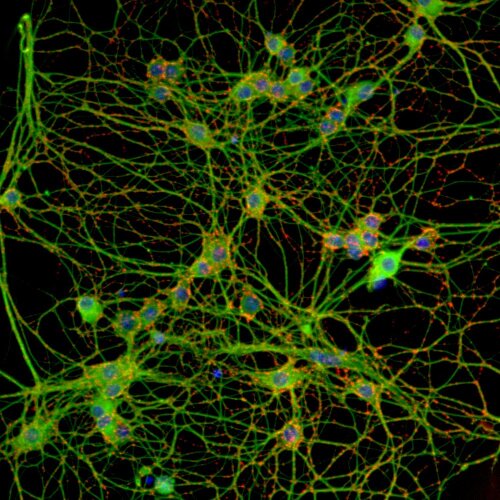
Neuro-immune communication in the gastro-intestinal tract is a key process involved in normal intestinal physiology as well as in intestinal disorders, ranging from inflammatory bowel diseases to functional disorders such as irritable bowel syndrome. G-protein coupled receptors are important drug targets and possible mediators of this neuro-immune communication. We are curently investigating the role of Mas-related G-protein coupled receptors (MRGPR’s). Gastro-intestinal inflammation causes marked expressional changes of MRGPR members in the enteric nervous system (ENS) and mucosal immune system. Using a broad repertoire of techniques, ranging from in vitro cell culture to advanced microscopy, we are now further unraveling the functional role of these receptors as underlying players in the pathology of gastro-intestinal disorders, with a focus on translation to the human gasto-intestinal tract.
AAV transduction in neurogastroenterology
Viral vector transduction in neurogastroenterology
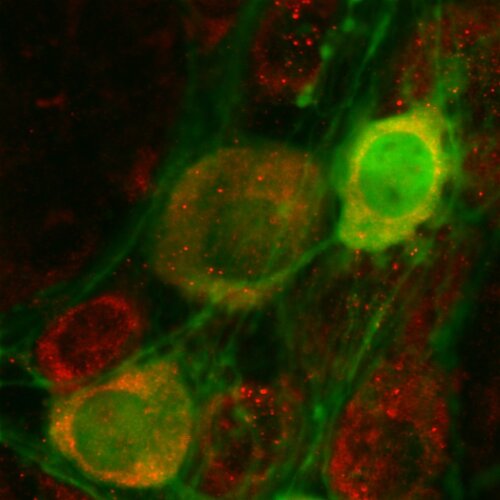
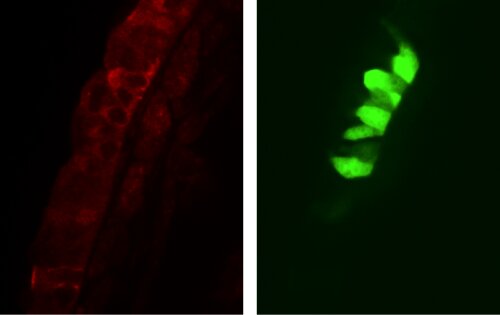
Despite the success of viral vector technology in the transduction of the central nervous system in both preclinical research and gene therapy, its potential in neurogastroenterological research remains largely unexploited. Adeno-associated virus transduction with genetic encoded indicators will make it possible to further unravel the functioning of the enteric nervous system (ENS) through advanced microscopy such as live cell imaging. In a later stage this knowledge will be used to genetically manipulate specific subtypes of enteric neurons in preclinical research. This will lead to a better understanding of the pathogenesis of gastro-intestinal disorders resulting from often subtle defects in the enteric innervation.
The enteric nervous system: a new entry route for neurodegenerative processes such as Alzheimer's disease in the brain
Alzheimer’s disease (AD) currently affects 1 in 9 individuals over 65 years of age but its prevalence will only rise against the background of a steadily greying population. With no cure currently available and diagnosis relying on the assessment of late-stage cognitive decline, it is imperative that novel early medical entry points are explored through original fundamental research.
Recent insights suggest that the gut may be a vulnerable node for amyloid-driven neurodegeneration. That is why we want to define the origin, entry routes and spreading behaviour of amyloid proteins in the enteric nervous system (ENS). Using innovative imaging technologies and well-defined molecular analyses, we will shed light on a novel gut-brain relationship with relevance for future (pre-)clinical research.
As the gut represents a unique, minimally invasive window to assess neuropathology, our work may spark the development of early biomarkers that directly report on disease progression in AD-patients. Moreover, confirming the notion that microbial-derived amyloids could represent a putative trigger for pathology may cause a paradigm shift for AD therapy.”
Pulmonary NEB's as a potential stem cell niche
The neuroepithelial body microenvironment as a potential stem cell niche in the airway epithelium
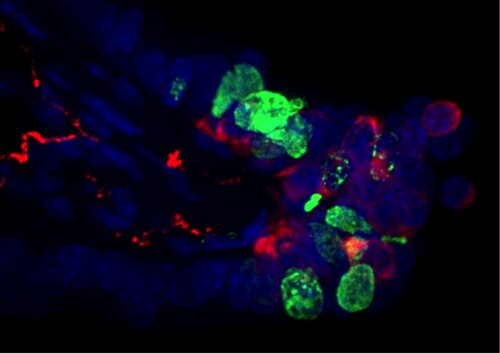
Literature data point out that the microenvironment (ME) of pulmonary neuroepithelial bodies (NEBs) is important during embryonic development and for adult airway epithelial repair after severe injury. NEB cells have also been reported to be the origin of cancer cells in a mouse model for small cell lung carcinoma (SCLC). Although the pulmonary NEB ME has been suggested to act as a (cancer) stem cell niche under these circumstances, little is known about its potential stem cell characteristics healthy postnatal lungs. The NEB ME consists of highly innervated groups of pulmonary neuroepithelial endocrine cells that are specifically covered by Clara-like cells, a special type of Clara cells with supposed stem cell characteristics. We developed a laser microdissection (LMD) based method that is compatible with high-end PCR techniques to selectively isolate the NEB ME from the airway epithelium and compare gene expression with control airway epithelium. A mouse model of lipopolysaccharide(LPS)-induced transient acute lung injury has been created to explore changes in gene expression of the NEB ME, compared to healthy controls, in order to further unravel the stem cell capacities of the NEB ME.
Dipeptidyl peptidase in acute lung injury
Dipeptidyl peptidases as potential therapeutic target in acute lung injury
Acute lung injury (ALI) describes a clinical syndrome of severe acute respiratory failure, caused by an inflammatory response of the lung to a prior insult, and for which no effective treatment is available. Previous research has indicated the potential involvement of dipeptidyl peptidases (DPPs) in ALI. DPPs are a family of enzymes that are capable of cleaving aminoterminal dipeptides from oligopeptides, causing changes in the biological activity of the substrates. The precise role of DPPs in the healthy lung and in the pathogenesis and pathology of lung inflammation is however poorly understood today. We want to further explore the expression and roles of DPPs, based on mouse models for infectious and non-infectious ALI and human lung samples, and gain insight in the therapeutic potential of DPP-manipulation in ALI. Immunohistochemistry and laser microdissection with subsequent quantitative PCR analysis, will be used to study the expression of DPPs and DPP-substrates in different cell types of the lung. Live cell imaging in an ex vivo lung slice model will be used to assess the effect of DPP-inhibition.
This research line is supported by a GOA BOF 2015 grant and the University of Antwerp research consortium that is involved.
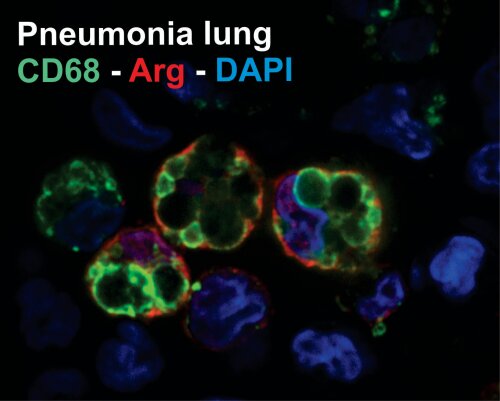
Molecular characterization of pneumonia
Molecular characterization of VAP and other types of pneumonia
Acute pneumonia causes the greatest morbidity and mortality amongst all infections. Our group has recently established different animal models of pneumonia including acute pneumonia model, ventilator associated pneumonia model, cystic fibrosis model and non-infectious acute lung injury models such as bead obstruction en mechanical ventilation models. We utilize these models to study disease pathogenesis of different types of pneumonia on the cellular and molecular level using the following techniques.
- Transcript analyses on qPCR and RNA-seq on whole lung, blood and isolated cells
- Magnetic-bead multiplex ELISA using Luminex technology for quantification of specific immunological targets
- Immunohistochemistry and immunocytochemistry using high-resolution confocal-microscopy for cellular characterisation
- In vivo animal monitoring using whole-body lung plethysmography and bio-imaging methods
- In vitro stress and virulence pathways identification and characterisation of prokaroytes using Orbitrap mass spectrometry and other spectrometric approaches
- Biomarker discovery on animal model and patient samples using state-of the art proteomics, metabolomics and lipidomic screens
Our close collaboration with the Laboratory of Medical Microbiology (VaxInfextio) and with the Intensive Care Unit of our university hospital UZA gives us a unique opportunity to help us answer clinically relevant questions in a translational context.
Stroke and stroke-related penunomia
Stroke and stroke-related penunomia
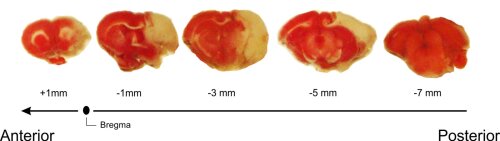
Cerebrovascular accident, or stroke, is the second most important cause of mortality worldwide. Stroke patients show increased susceptibility towards developing of infectious complications such as pneumonia.
The major determining factor for this increased susceptibility towards infections is the development of post-stroke immune suppression. Through various mechanisms, not yet fully understood but known to be originating from overactivity of the sympathetic nervous system and the HPA-axis, the immune system is downregulated after stroke resulting in lymphocyte apoptosis and leukopenia. In this project, we study the behaviour of T-lymphocyte subsets and specific cytokine profiles in the brain and periphery after stroke in an experimental animal model of ischemic stroke (MCAO model) by immunohistochemical and molecular approaches (such as multiplex ELISA and RNA transcript analyses). In collaboration with UZA-Neurology (Prof. Patrick Cras, Dr. Laetitia Yperzeele ), we are also validating our findings on stroke patients for translational purposes.